Do You Need a Biopsy for Alopecia?
There’s a saying in the functional medicine community, “Don’t guess, test.”
And yes, testing can reveal imbalances previously unknown. I like to see a combination of serum, urine, and fecal testing for a few values. Like an underactive thyroid. Or an infection like H. pylori. Or anemia. Or low metabolized cortisol. Or high SIgA (secretory IgA). Or high fasting insulin.
While I’m pretty savvy about functional testing, including the appropriate reference ranges (which is a huge consideration, as conventional ranges are often outdated, leading to underdiagnosis), I’m not a licensed medical provider therefore not qualified to diagnose anyone with anything.
One type of testing that many of my alopecia clients wonder about getting a scalp biopsy.
These include:
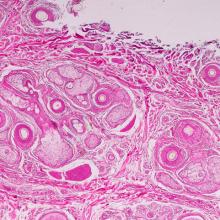
- Punch biopsy, which is extracting a sample of skin with a circular tool
- Shave biopsy, which is the shaving of a sample with a razor blade
Go here for my ebook, Hair Loss: It’s Reversible without Drugs, Creams, Injections, and Steroids >
Go here to check out my year-long Reversing Alopecia Roadmap course >
To what end?
While I understand the desire for a label or “official” diagnosis, it makes me scratch my head (no pun intended) that providers offer biopsies because while they claim that they’ll help to determine an “accurate diagnosis,” they rarely change their treatment plan based on the results.
“Alopecia” is the medical definition for hair loss of any pattern. Many providers refer to “alopecia” specifically as patchy or total loss, but strictly speaking, the term refers to any pattern of inordinate shedding.
Upon biopsy analysis, many doctors will say, “You have alopecia.” Um, right.
This leaves the patient often bewildered because they think, “Well yes, I knew I was losing hair. This is why I made the appointment. Now what?”
To me, biopsies aren’t a good use of time or money because for the most part, doctors (dermatologists, sometimes endocrinologists) will say, “You’re just stressed.”
Or they’ll reflexively write prescriptions for the same ol’ drugs that have never worked for lasting hair growth and long-term reversal of alopecia. (How alopecia ever got relegated to the dermatological community still has me stumped.)
Maybe it’s a Rogaine (Minoxidil) prescription. Or Finasteride. Or Spironolactone. Or a JAK inhibitor.
Don’t get me started on JAK inhibitors.
Finasteride and Spironolactone should never be administered without a full androgenic hormone workup. And they haven’t been shown to work well in women.
Finasteride is a 5-alpha reductase inhibitor and DHT blocker, but doctors too often write a script for it without doing testing to determine if someone has DHT to block in the first place! Or whether they’re already high in testosterone. Oy.
And if someone is sitting in the 5-beta reductase pathway vs. the 5-alpha, this prescription will do nothing. (I offer specific testing (DUTCH) that determines if someone is in 5α or 5-β and also measures your androgenic hormones, including DHT, DHEA, testosterone, and testosterone metabolites. Reach out if you’d like this test.)
Not to mention, according to a nutritional bombshell from the Journal of Chemistry and Biodiversity, fatty acids (EFAs) block 5α-R and the conversion of testosterone to DHT. EFAs have been said to work better than Finasteride! Oy oy.
Spironolactone is an androgen blocker. Again, you need to test your androgens before even thinking about taking it.
Additional analyses for the scalp and follicles are:
- Trichogram: microscopic examination of hairs
- Dermoscopy/trichoscopy: follicle analysis through magnification
- TrichoScan®: software-based, digital analysis
But what are we really testing here?
Providers are generally looking for:
- Inflammation
- Miniaturization
- Infection
- Follicular damage
But what are the root cause approaches to these conditions so that people can see lasting improvements, not temporary progress with the risk of pharmaceutical side effects?
Let’s take a closer look at all of them.
Inflammation
There are many reasons the follicles can be inflamed, like a fungal or bacterial infection, which is common with alopecia. Or high insulin. Or cortisol overproduction (many with alopecia have an extra adrenal cortisol receptor site in their follicles). Or stagnant lymph.
Another common cause of scalp inflammation is seborrheic dermatitis, which is thought to be autoimmune in nature.
Is an “anti-inflammatory” corticosteroid going to help with any of this long-term? No. And in fact, corticosteroids can also alter your androgen profile, which can make things worse in the long run.
Miniaturization
Miniaturization is hair follicle restriction, causing thinner hairs overall. This is most often seen with the androgenic alopecia pattern, sometimes called androgenetic alopecia or FPHL (female pattern hair loss) in women. Women with PCOS often have androgenic alopecia.
While many doctors and medical journalists will claim that androgenic alopecia is “irreversible or only partially reversible,” according to a 2003 American Academy of Family Physicians article, Alopecia in Women, “Because androgenic alopecia is an aberration of the normal hair cycle, it is theoretically reversible.” They do clarify that this may not be the case if it’s “advanced.”
Infection
Again, a fungal or bacterial infection is common with alopecia. But what is the infection specifically? Is it fungal? Bacterial? A combination? Is it Demodex mites?
Get this: Mites can cause inflammation or altered hormone metabolism (increased DHT) that leads to androgenic alopecia. Oy oy oy.
Bacterial infections are often treated with oral antibiotics, but that can set people back by way of microbiome/gut disruption, which is a big consideration given that 70-80% of our immune system is in our gut.
There are several phytomedicine combinations (herbs) that are both anti-fungal and anti-bacterial. Most often, by the time a pathogenic infection has taken up residence in the follicles, it’s systemic, meaning, it’s a good idea to treat both internally as well as topically. Remember, reversing alopecia is an inside job.
A good reason to consider a biopsy is a possible mite infestation, although this can also be diagnosed via dermoscopy. Tea tree oil is a treatment for follicular mites.
Follicular damage
This is most often seen with untreated cicatricial (scarring) alopecia and scalp ringworm (tinea capitis). While I don’t generally work with people with cicatricial alopecia, lasers and the herb gotu kola have been shown to be helpful. Tinea capitis tends to respond well to an anti-fungal approach, both internally as well as topically.
Last but not least…
What’s not in the above list but that can be analyzed with a biopsy is mast cell activity in the scalp. This topic is beyond the scope of this post, but degranulated mast cells are one of the primary drivers of alopecia; many with alopecia have mast cell activation disorder (MCAD), also known as mast cell activation syndrome (MCAS).
Mind you, you don’t have to get a scalp biopsy to know if it’s one of your root causes. If you have a history of chronic allergies and histamine issues, according to Dr. Greg Plotnikoff, it’s likely you have unstable mast cells. While allergies and histamine overproduction aren’t the only tip-off, they’re a big one.
Do you need a label?
I sleuth out ALL of these potential root causes—and more—with my clients and Reversing Alopecia course participants. While I don’t claim to be all things to everyone, for the most part, I feel that the same hair growth strategies can be helpful no matter what the outcome of biopsies or other “scalp analysis.”
Do you need a diagnosis to heal? Or are you spending time and money to get a label with no real direction—and possible pharmaceutical side effects that will leave you worse off than before?
I don’t want to discourage anyone from working with a trusted medical professional and there’s certainly no harm in getting a biopsy. Just understand that alopecia is multifactorial and while that may seem overwhelming, everything works together. I know it sounds cliché.
But at some point, my clients and course participants start to see everything (immune system, hormonal system, digestive system, lymphatic system, etc.) as…a system…and that brings about a lot of comfort, motivation, and understanding that…
“Your body’s ability to heal is greater than anyone has permitted you to believe.”
Add comment